Introduction
The global prevalence of gastroesophageal reflux disease (GERD) is estimated to be around 15%. According to the latest Global Burden of Disease Study (GBD), the total burden of GERD has surged by 77.53%, rising from 441.57 million cases in 1990 to 783.95 million in 2019.1 While overall incidence in Asia was reported to be lower, regional variations exist with India showing a notably higher prevalence. Major population-based studies in India indicate a GERD prevalence of approximately 10%, a figure that was likely increasing due to changing lifestyles and rising obesity rates.2, 3 A meta-analysis by Rai et al. reported a pooled prevalence of 15.6% for GERD in the Indian population.3
Nocturnal heartburn affects up to 25% of the general population with GERD and was known to cause sleep disruption, further impacting quality of life and psychomotor performance.4 Moreover, it may elevate the risk of developing conditions such as cardiovascular disease, esophageal adenocarcinoma and obstructive sleep apnea syndrome.5 The introduction of proton pump inhibitors (PPIs) revolutionized GERD treatment. However, 30% of GERD patients receiving standard PPI doses continued to experience symptoms, highlighting a significant therapeutic gap.6 Prokinetics, known for enhancing gastrointestinal motility, emerged as an alternative approach. Initially recommended as first-line treatment for functional dyspepsia patients with postprandial distress syndrome, prokinetics gained attention in GERD management.7 Several studies demonstrated that combining prokinetics with PPIs provides additional benefits in global symptom improvement for GERD patients, compared to PPI monotherapy.8, 9, 10, 11
Rabeprazole, a second-generation PPI, covalently binds to and inactivates the gastric parietal cell proton pump (H+/K+-ATPase).12 This mechanism effectively inhibits gastric acid secretion, making rabeprazole a potent treatment for gastrointestinal ulcers and GERD.13 Compared to omeprazole, the prototypical PPI, rabeprazole demonstrates 2 to 10 fold greater anti-secretory activity in vitro, enhancing its efficacy in managing GERD symptoms and promoting ulcer healing.14 Domperidone, a widely recognized antiemetic, serves as a prokinetic agent by blocking dopaminergic receptors, increasing lower esophageal sphincter pressure and stimulating gastric motility. By accelerating gastrointestinal peristalsis, domperidone effectively improves gastrointestinal function. 11, 15
This combination therapy approach addressed the limitations of PPIs alone, offering a potential solution for patients with refractory GERD symptoms. The synergistic effect of PPIs and prokinetics suggested a more comprehensive treatment strategy, targeting both acid suppression and motility enhancement in GERD management in clinical studies. So, this survey aimed to gather insights into GERD management in India, focusing on the prescription practices and effectiveness of combining rabeprazole with domperidone for nighttime heartburn. The survey findings help to understand the perceived efficacy and safety of this combination in managing nocturnal GERD symptoms.
Materials and Methods
We carried out a cross sectional study among clinicians specialized in GERD management in the major Indian cities from June 2023 to December 2023.
An invitation was sent to leading clinicians in managing GERD in the month of March 2023 for participation in this Indian survey. About 46 gastroenterologists from major cities of all Indian states representing the geographical distribution shared their willingness to participate and provide necessary data. Clinicians had the flexibility to skip questions they chose not to answer. They were instructed to complete the survey independently, without consulting colleagues. All participants provided written informed consent prior to the initiation of the study. The questionnaire booklet titled RARE (Rabeprazole + Domperidone in night time heart burn in GERD) study was sent to the physicians who were interested to participate. The RARE study questionnaire comprised 24 questions focused on gathering various aspects of GERD management, including patient demographics and prevalence, clinical challenges, treatment preferences, efficacy of different treatment combinations, patient adherence, use of clinical guidelines, associated comorbidities, risk factors and patient education methods.
Statistical analysis
Descriptive statistics were used to analyze the data. Percentages were utilized to depict the distribution of categorical variables, displaying both the frequency and corresponding percentages for each variable. Microsoft Excel 2013 (version 16.0.13901.20400) was employed to create graphs and pie charts, visually representing the distribution of these variables.
Results
A total of 46 clinicians participated in the survey. According to 39% of clinicians, 31-40 cases of GERD patients per month report nighttime heartburn in their clinical practice, while another 39% of clinicians observe 21-30 such cases monthly. Most clinicians (54%) reported that the age group 45-60 years experiences the most complaints of nighttime heartburn in GERD patients. Majority of the clinicians (41.30%) reported that hypertension is the most common co-morbid condition observed in GERD patients who experience nighttime heartburn. Majority of clinicians (43.48%) indicated that an improper diet is the most significant factor increasing the risk of GERD in their clinical practice. Majority of the clinicians (41.30%) preferred individual one-to-one sessions for educating patients with GERD. Majority of clinicians (45.65%) reported that ensuring patient compliance with the regular consumption of medication is the most challenging aspect in managing GERD.
Around 48% of experts preferred using the American College of Gastroenterology (ACG) guideline for GERD care. Approximately 46% reported that a lack of patient education is the primary factor associated with patient non-adherence to medication for GERD. Most clinicians (65.22%) preferred pellets or capsules as the dosage form for PPIs. According to 47.83% of clinicians, 21-30% of GERD patients require combination therapy for effective management. According to 33% and 30% of clinicians, fixed drug combinations in GERD are advantageous because they improve patient adherence and offer better tolerability. More than half of clinicians (52.17%) recommended medication for nighttime heartburn at night. A significant proportion of clinicians (63.04%) decided the PPI to be prescribed for nighttime heartburn based primarily on their clinical experience. Majority of the clinicians (67.39%) rated the technologically superior PPI with acid-resistant pellet technology (ARP2) as excellent for treating nighttime heartburn in GERD.
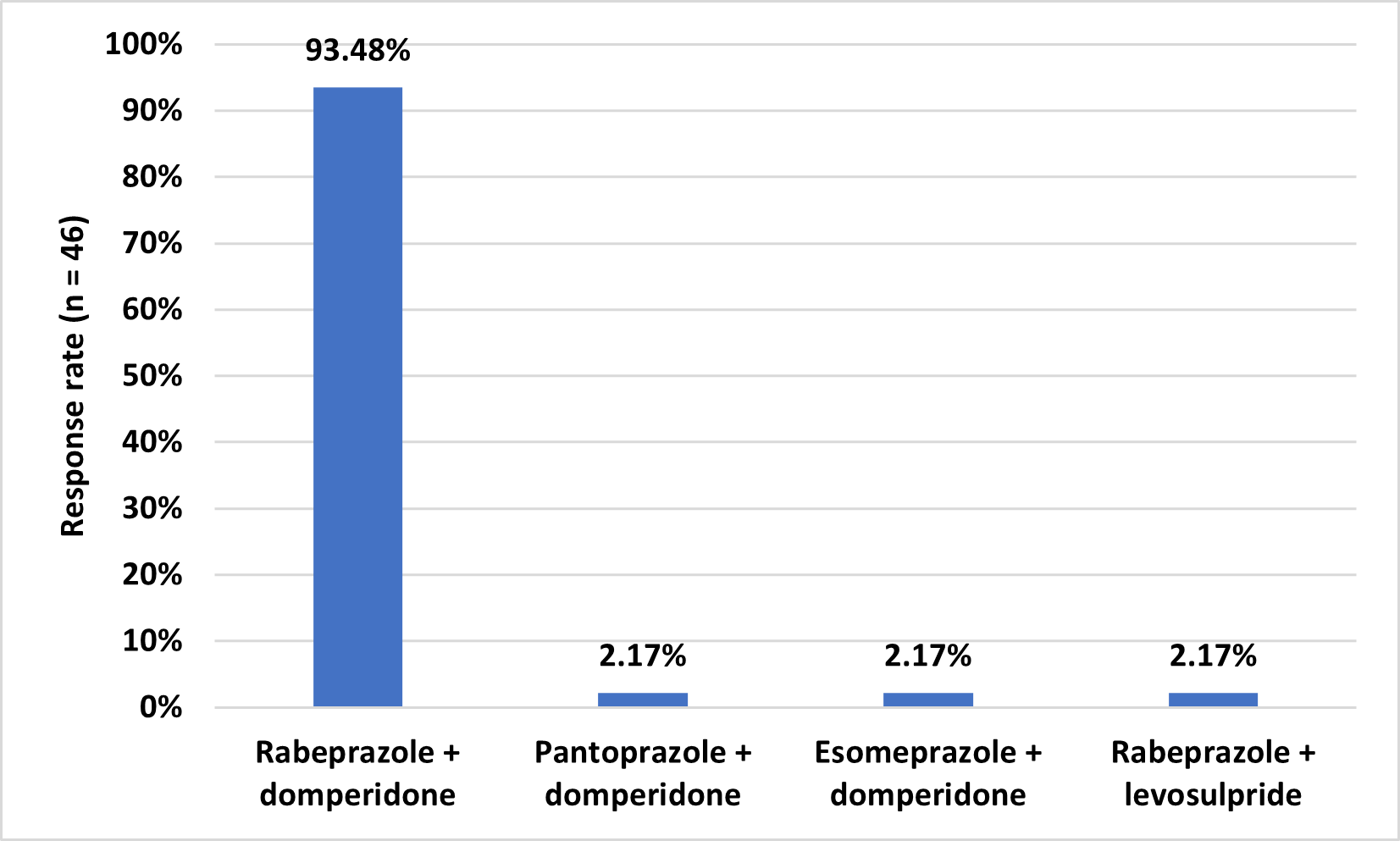
Most of the respondents (95.65%) preferred rabeprazole for its longer action in managing nighttime heartburn in GERD (Table 1). A significant number of clinicians (95.65%) preferred prescribing the combination of rabeprazole and domperidone for managing nighttime heartburn in GERD (Table 2). Majority of the clinicians (89.13%) stated rabeprazole + domperidone is more effective in treating nighttime heartburn with GERD compared to other PPI combinations (Figure 1). Majority of the experts (93.48%) preferred that the combination of rabeprazole and domperidone provides the fastest relief for nighttime heartburn in GERD (Figure 2). Approximately 54% reported that <5% of their patients had switched from rabeprazole + domperidone to another PPI due to lack of efficacy or adverse effects.
Table 1
Distribution of response to preferred proton pump inhibitor for longer action in nighttime heartburn in GERD
|
Proton pump inhibitor |
Response rate (n = 46) |
|
Rabeprazole |
44 (95.65%) |
|
Pantoprazole |
1 (2.17%) |
|
Esomeprazole |
1 (2.17%) |
|
Omeprazole |
0 (0%) |
Table 2
Distribution of response to typical prescription for nighttime heartburn with GERD
|
Drug combination |
Response rate (n = 46) |
|
Rabeprazole + domperidone |
44 (95.65%) |
|
Pantoprazole + domperidone |
1 (2.17%) |
|
Esomeprazole + domperidone |
1 (2.17%) |
|
Omeprazole + domperidone |
0 (0%) |
Figure 1
Distribution of response to efficacy comparison of rabeprazole + domperidone with other PPI combinations in treating nighttime heartburn in GERD
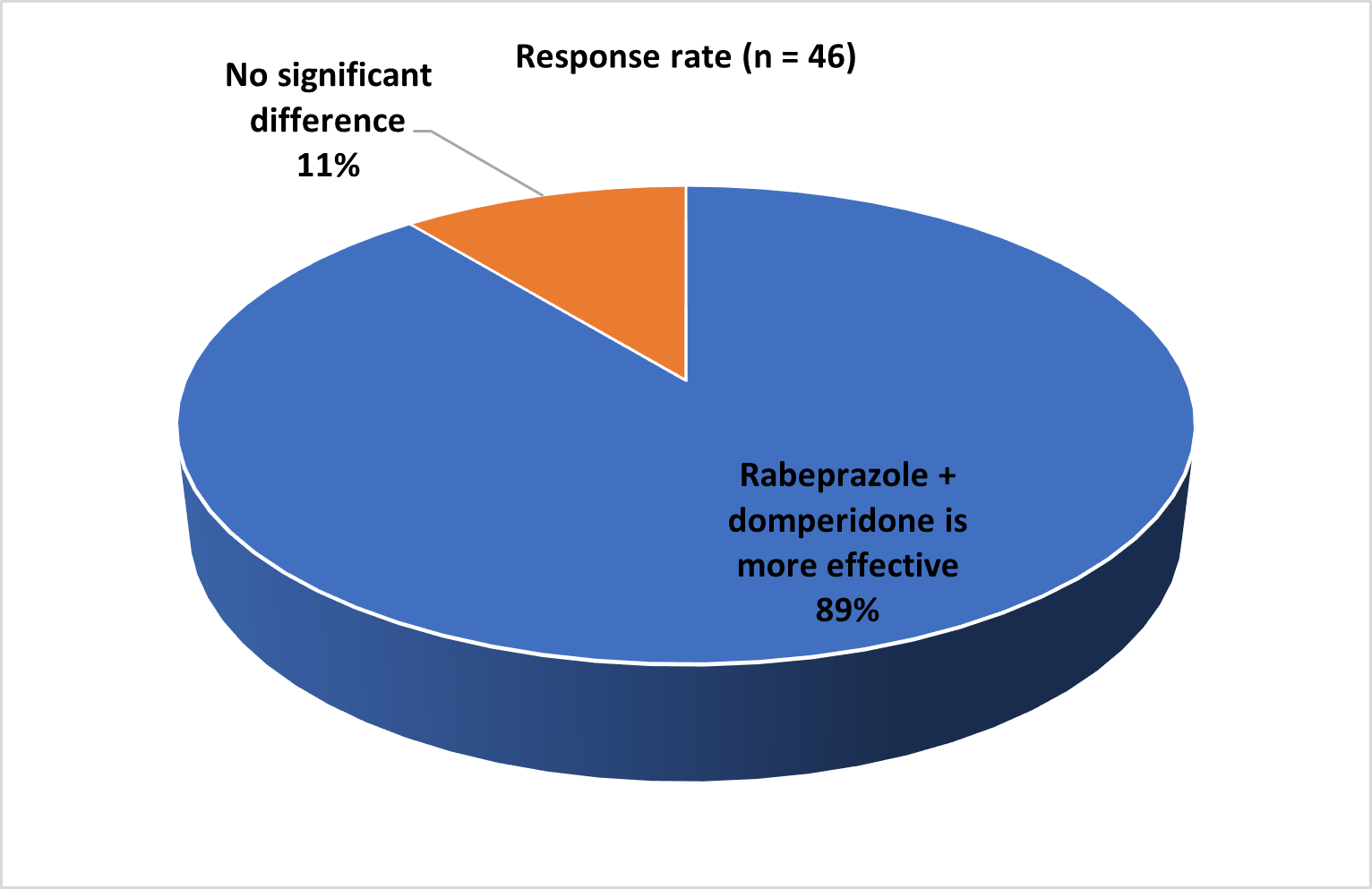
Figure 2
Distribution of response to drug combinations providing the fastest relief for nighttime heartburn in GERD
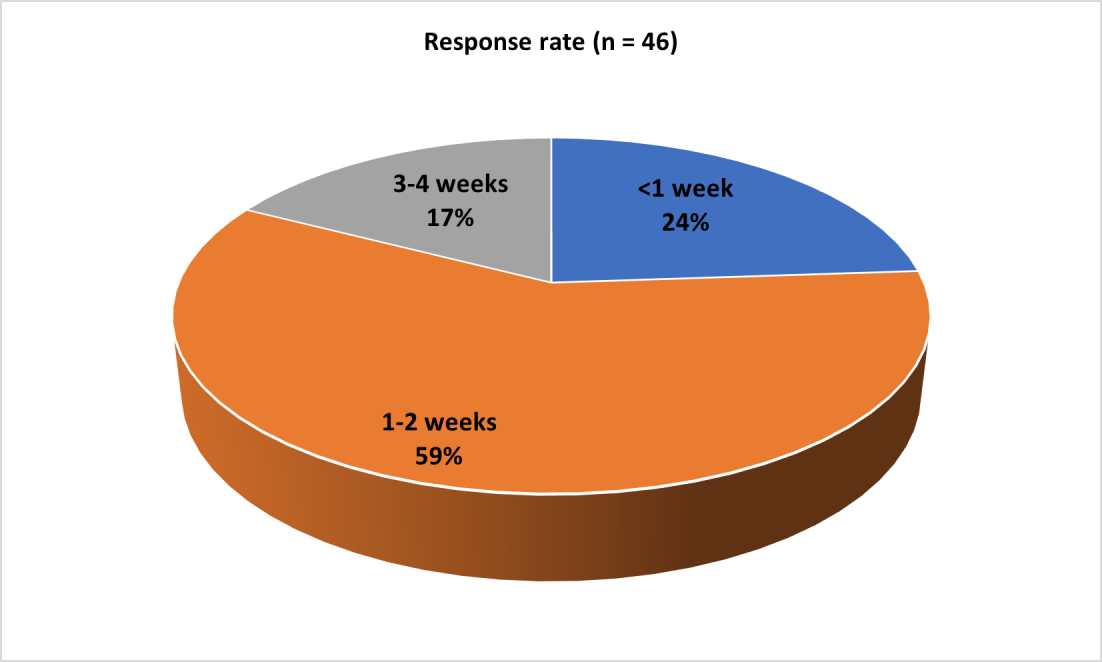
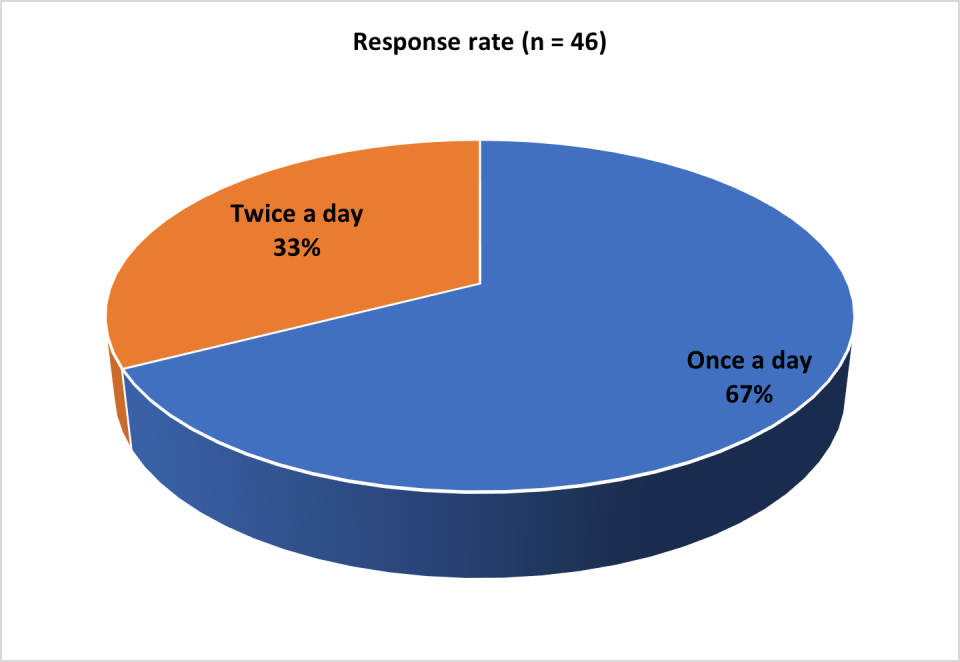
The majority of the clinicians (41.30%) reported that 40-60% of their patient’s experience relief from nighttime heartburn in GERD after using the rabeprazole plus domperidone combination. Additionally, another 41% of clinicians observed that 60-80% of patients experienced relief with this treatment (Table 3). Most clinicians (67.39%) recommended that patients with nighttime heartburn in GERD receive rabeprazole plus domperidone once a day (Figure 3). Around 59% of the experts reported that their patients felt relieved from nighttime heartburn in GERD within 1-2 weeks after starting the rabeprazole plus domperidone regimen (Figure 4). Approximately half of the respondents (50%) indicated that they were most likely to prescribe Helirab D to their patients due to the advantages of ARP2 Technology (Table 4). Most clinicians (60.87%) reported that the typical prescribed duration of treatment with rabeprazole plus domperidone for patients with nighttime heartburn in GERD is 4 weeks.
Table 3
Distribution of response to proportion of patients who experienced relief from nighttime heartburn in GERD with rabeprazole + domperidone
|
Proportion of patients |
Response rate (n = 46) |
|
20-40% |
2 (4.35%) |
|
40-60% |
19 (41.3%) |
|
60-80% |
19 (41.3%) |
|
80-100% |
6 (13.04%) |
Figure 3
Distribution of response to recommended frequency of rabeprazole + domperidone for nighttime heartburn with GERD
Discussion
The current study provides a framework for understanding the clinician’s perspectives on GERD management, particularly focusing on night-time heartburn and may offer valuable insights for improving patient care and treatment strategies. The survey results indicate a strong preference among clinicians for rabeprazole, particularly in combination with domperidone, for managing nighttime heartburn in GERD. This preference is likely due to rabeprazole's longer duration of action and the synergistic effect when combined with domperidone. A systematic review and meta-analysis by Jung et al., which included 16 randomized controlled trials (RCTs) with a total of 1,446 participants, reported that the combination of prokinetics with PPI treatment was more effective than PPI alone in patients with GERD.16 The synergistic action of rabeprazole and domperidone addresses both acid secretion and gastrointestinal motility, making this combination particularly effective for patients with GERD, especially those experiencing nighttime heartburn.
Majority of the current survey clinicians preferred rabeprazole in managing nighttime heartburn in GERD, which aligns with previous studies demonstrating similar effects. The POWER GERD Study by Lawate et al. demonstrated that rabeprazole effectively provided rapid and sustained relief for both daytime and nighttime GERD symptoms in patients with moderate to severe GERD.17 Several other clinical trial studies also reported the effectiveness of rabeprazole in the reduction of nighttime heartburn in GERD patients.18, 19, 20 The combination of rabeprazole with domperidone, a prokinetic agent, appears to enhance the therapeutic effect, as supported by most of the clinicians reporting greater efficacy compared to other PPI combinations. A systematic review and meta-analysis of RCTs by Zamani et al., evaluated 11 studies with a total of 841 participants, reported that the combination of domperidone with a PPI was generally safe and more effective in treating GERD compared to PPI alone.11
With a significant number of clinicians noting the fastest relief from the rabeprazole-domperidone combination, this represents a notable clinical advantage. This quick response may contribute to improved patient compliance and satisfaction. The majority of clinicians observed relief in 40-80% of patients within 1-2 weeks of treatment initiation, suggesting a high rate of clinical success. The once-daily dosing regimen recommended by most clinicians aligns with convenience, potentially enhancing adherence. Additionally, the preference for Helirab D (a combination of rabeprazole and domperidone) by 50% of clinicians due to its ARP2 technology suggests that formulation advancements play a role in prescription decisions. This technology may offer benefits in terms of drug delivery or absorption, though further research is needed to confirm its clinical significance.
An open, prospective study conducted among Indian subjects by Shahani et al. assessed the efficacy and tolerability of rabeprazole and domperidone combination in treating GERD among 50 patients. Daily administration of the combination for up to 4 weeks resulted in significant symptom improvement, with noticeable effects within 2 weeks and additional gains over the full period. The treatment was well tolerated, with 94% of patients receiving excellent or good relief and 86% rating it as good or excellent. The study concluded that rabeprazole and domperidone combination not only effectively alleviated GERD symptoms but also improved patients' quality of life.21 Another open-label, multicenter study that enrolled 2,579 patients showed that an 8-week treatment with 20 mg of rabeprazole once daily significantly and rapidly reduced the severity of both daytime and nighttime heartburn while also improving symptoms of regurgitation and belching.18
This survey provides valuable insights into clinicians' preferences and experiences with rabeprazole and domperidone combination therapy for nighttime heartburn in GERD. It highlights the perceived efficacy and convenience of this treatment. The high rate of clinical preference and reported patient relief suggests that this combination may offer a promising treatment option for managing nighttime GERD symptoms. A major strength of the survey is the use of a meticulously designed and validated questionnaire for collecting expert data. However, the reliance on clinician-reported data rather than direct patient outcomes or randomized controlled trials limits the robustness of these findings. The smaller sample size of 60 clinicians may not represent the broader medical community and regional variations in practice patterns may exist. The lack of a specified sample size, potential selection bias and absence of comparative data with other treatments further constrain the generalizability of the results. Additionally, the survey does not address long-term efficacy, safety profiles, or patient-reported outcomes, which are crucial for a comprehensive evaluation of any treatment regimen. While these findings provide a useful starting point for understanding real-world clinical preferences, they should be interpreted cautiously and validated through more rigorous, patient-centered research methodologies.
Conclusion
The survey results demonstrated a strong clinical preference for the combination of rabeprazole and domperidone in managing nighttime heartburn in GERD. This combination appears to offer advantages in terms of efficacy, speed of onset and patient relief. The once-daily dosing regimen and formulation technology (ARP2) may contribute to its favored status among clinicians.